Skip to content
The current and growing scale of Social Prescribing activity across the country An estimate of the success of activity in providing a successful referral into physical exercise A broader perspective on community referral processes An overview of the different measurement tools that are used in association with Social Prescribing Some conclusions, therefore about how to best position within this broader set of considerations.
On average, each SPLW tends to support a caseload of about 40 people at any one time They tend to “turnover” their caseload approximately every two months (meeting people 3-4 times in that time period perhaps) This therefore equates to an annual caseload of about 200-240 people in a year per SPLW (allowing some time-off for leave and training etc).
Firstly, arguably, there is better evidence for the positive impact of physical exercise on preventing health conditions, rather than exercise as a “treatment” for existing concerns or issues. In particular, for example, the impact on preventing escalating risks in cardiovascular disease, stroke, diabetes, bone fractures and a very headline level mortality from all causes. The GP-led referral process targets people who, rightly or wrongly, have decided to seek support from Primary Care and hence their own view is that they need and want treatment. For them the discussion is about treatment rather than prevention, and physical exercise as a treatment for their concerns is less likely to be successful (than prevention would have been years earlier)Secondly, people have fewer barriers to overcome where they are found earlier in any health pathway and hence they will be more likely to engage, compared to a stage where they have plucked up courage to seek support from a GP Driving behaviour change is easiest where there is speedy feedback in terms of evidence of the impact. People may make quicker progress where there are fewer barriers to overcome and hence they may feel encouraged / incentivised to continue, where they can see evidence of the impact. Low level Mental Health Those with finance and housing concerns People worried about controlling their behaviour - be that substance related or about anger issues People with seeking support and access to the right type of reasonably-adjusted pathways and offers. There may be some changes to the expectations around caseload and productivity for . It is not guaranteed that increased throughput will drive increased volume of referrals for exercise; the cohort being supported tend to be anxious and moving from say 4 conversations to only 2 may not provide the time to gain their confidence and motivate someone to start to take exercise.The SPLW market is highly fragmented, in terms of the cultural leadership and decision-making. There may be a very high volume of people to influence to change the behaviour of each SPLW, with each PCN employing 1-2 SPLW on behalf of an average of 3-4 GP practices.There are a high number of other community-based referral processes that might be targeted simultaneously. Firstly, the evidence demonstrates that the greatest impact on health outcomes is where exercise is alongside other behavioural change (most notably diet); Secondly and more importantly, people are within these referral pathways for a reason; what they are seeking is short-term respite from often fairly debilitating concerns. In this context, any push to use social prescribing to increase referrals into exercise will need to be considered sensitively to ensure it can be positioned as something that people will engage with as an opportunity and discussion.Finally, change being driven within the processes is going to create increased pressure on outcomes and productivity and hence it may be better to position generically as part of Open Data rather than trying to explain that there are different Open Standards and that not all software products can work with them all. Adopting open data will have productivity benefits and therefore is well aligned to the emerging concerns about performance. This level of complexity may be a hard set of messages to promote across the very fragmented world where there is a lot of competing marketing and transformation pressures.
How many cases are being handled, to establish some insight into performance How many times are people being successfully referred into non-medical community support (this is the core measure of success in terms of something that a SPLW can held to account to enable - in that it would be very difficult to motivate an SPLW where they are held accountable for their clients to achieve better health outcomes) Any qualitative feedback on the SPLW or the process – where that might be complaints or complements – in other words some consideration of quality of that process and service (the service being the act of making the links). Put simply was the process helpful and if so (or if not) then why? There is no process for capturing evidence of attendance at services / activities – it is all anecdotal. It is also arguably counter-productive – the patients are all vulnerable and mostly anxious people lacking confidence; informing them that the information will be used to monitor / measure their improved health runs the risk of discouraging them from participating. Where there is any correlation between this anecdotal attendance and improved outcomes, there is no evidence these correlations are causal. In reality, a myriad of other factors (diet, other events in someone’s life such as bereavements, relationship breakdown, new births, changes to finance / employment status etc) are likely to have a greater impact on better reported outcomes and there is no process to disaggregate the impact of these other more important factors from the impact of either the support or an activity or group attended.The sample size of the data is often very small and doesn’t represent the whole activity (so if ten people report fantastic outcomes, but 200 people attended the activity, but did not report any feedback, then the 10 pieces of positive feedback cannot be taken as broader evidence – other than feedback to those 10 individuals that for them they are reporting feeling better / happier). Is the sample size representative of the broader population? For example, the information may often relate to specific cultural groups and hence this must be factored into any evaluation. The data captured is not reliable and is also a very short timeframe snapshot. Where there is interest in longer-term behavioural change, then there would need to be the right long-term evaluation. Many of the SPLW services interviewed do undertake some follow-up assessments, but again these are at best ad hoc and offer no reliable data. The measures are captured across an enormous breadth of service types, including activity, but also befriending, benefits advice and perhaps tenancy advice and support. Given this breadth of scope, it is not clear how the information could be used to determine any meaningful insight into the impact on outcomes of such a breadth of services and activities. Where judgements or evaluation is considered about whether a particular service is delivering better outcomes, then there should be caution about making the assumption that a yoga service, for example, in one town is comparable to another one in another town. Similarly, it is not possible to assume that a yoga session that worked well for someone with a particular set of conditions, could be appropriate and beneficial to people with different sets of conditions or risks Even if many of these statistical considerations can be addressed, it must not be forgotten that more often than not the “service” or activity (not the SPLW process) is often delivered by a charity at no or very little cost. This type of evaluation mechanism is better suited to the commissioning of multi-million-pound contracts than evaluating local charity service provision. There is a need to improve the operational management of Social Prescribing. The SPLW interviewed were all highly motivated and believe in the work that they do; it is undoubted that the emotional support that they give their clients is highly valued. What is questionable is how to make best use of this resource and perhaps there should be a sharper focus on handover and look to ensure that community services create a better set of welcoming processes to smoothly bring people into their service / activity There will be a value in locally capturing information about the accuracy of information that describes local services and whether there are service offers available locally that meet people’s needs. This will inform the ability to improve the process - in terms of identifying gaps or duplication geographically and in terms of service typesThe core purpose and hypothesis behind Social Prescribing is that where someone’s health is starting to in part be affected by a wider set of personal, behavioural and potentially emotional factors, then there is likely to be value in helping these individuals access relevant support from community services. Where there is a wish to evaluate that this is true, then this should be a tightly controlled, scientific study. At a simple level, being more involved in some appropriate, low-level befriending, hobby / interest or activity groups can surely only be a good thing; whether there is a need to evidence this is debatable, accepting that things have to be appropriate rather than inappropriate There may be an interest in going deeper and evaluating whether service a or service b (or c or d etc - the range of service is arguably limitless as there is such a breadth of service offers available) has a demonstrable improvement on conditions v, w (or x or y etc). This again should be a set of scientific evaluations and will need to account for the impact that other life changes or events have on someone’s improved health outcomes (as distinct from the impact of the service itself). This type of evaluation is probably not the work of an SPLW service, but more suited to research by Academic Health Networks, for exampleOf particular interest may be setting up pilots where individual patients themselves take personal responsibility to track their own health. There are a huge range of tools available to track health indicators through blood tests, VO2 max, weight, calories used etc, alongside perception measures of emotional happiness. This data is best positioned as belonging to a patient and for them to take on responsibility to track it for their own benefit. This might not be tagged to be able to evidence the impact of service a, b or c, but provides an opportunity to track whether people generally take better care of their health, where this is something that they can measure frequently. For example, an initiative could request people attending a 40 year old health check to monitor their own health compared to statistical average and track this for a period or perhaps 2 years and comment then solely on whether being able to measure it generally helped them change their behaviour. The evidence exists through research for anyone who wants to understand the impact of exercise, diet or substance abuse for example on health. The pilot would be to evaluate whether people are more motivated to change behaviour because they have access to tools to track their health and increased risk of things like cardio, diabetes, stroke.
 Numbers and Measures
Numbers and Measures
Open Data and Social Prescribing. The hypothesis is that Open Data will provide a richer, more reliable and broader set of information that will support Social Prescribers to encourage an increased number of patients to take up physical activity.
@OpenActive
The document sets out some headline information about:
@SP
@OpenActive
The information presented is based upon a limited set of data; narrow sample sizes will always provide information that will make any decisions difficult, as it represents limited and unscientific evidence. However, there is some emerging dialogue locally and nationally that there is a need for some evaluation of Social Prescribing. This paper simply plays back findings about what is currently being measured and offers commentary about where and how this research might move forward.
The Scale of Social Prescribing Activity
There are 1250 Primary Care Networks () across the country; each has an average of approximately 1.5 Social Prescribing Link workers currently. The ambition is that this may increase to nearer two by the end of the current calendar year. A PCN consists of 4 or 5 GP practices on average and covers a population of approximately 30-50,000 people. Each PCN has autonomy on how their will work. However, broadly the interviews across all of Pennine Lancashire, Southport, North Lincolnshire and one London Borough indicate the following:
@PCNs
@SPLW
What seems to be emerging, is some questioning about whether this level of productivity is too low. One of the GPs interviewed commented, when pushed, that there is a notable difference to their own workload in treating 30 people per day, which is 50% more than a “treats” in a month. The role of the SPLW is different and time is needed to build relationship and confidence with the client; any expectation that social prescribing can successfully refer 30 people per day to community services is deeply mistaken.
@SPLW
It seems appropriate, however, to predict that caseloads may increase slightly in the coming months. The table below offers a potential range of the total numbers of SPLW cases per annum. It is believed that these figures may err on the high-side – mainly because Pennine Lancashire, which was the biggest influence into these estimates, has had a number of SPLW trials in place for 5 years and hence have a more established team.
SP cases per annum
1800 SPLW nationally
250 cases per annum
450,000
2500 SPLW nationally
350 cases per annum
875,000
There are no rows in this table
The Structure of SPL Workers
It is important to recognise that each GP practice is an autonomous business. The process and approach that each PCN or GP practice takes to how their SPLW will work’ differs markedly. On top of that, there have been probably 1,000 SPLW recruited in the last 12 months, who have come from a variety of backgrounds with different experiences; this is not a homogenous set of processes and culture. Finally, it is also important to recognise that come April 2022, will have more freedom about how they invest certain funding; they can choose to invest funds into a range of roles across a PCN, which include physiotherapists, pharmacists, health and well-being coaches, occupational therapists and care co-ordinators (which is mostly about palliative care support). The informal estimate is that perhaps 30% of PCNs will cease to commission Social Prescribing Link Workers; there is of course a chance that this flexibility may change.
@PCNs
Social Prescribing is a “busy” market therefore, with a lot of initiatives and strategies emerging locally and nationally. Any ambitions to create change needs to consider these contextual factors.
@SPLW process and the ability to make referrals into physical activity
@SPLW
Through the interviews, it was clear that the likelihood that a SPLW would discuss or explore someone’s attitude to or interest in being more active varies enormously. One individual commented that this discussion had happened less than 3 times in the last 12 months, where for another SPLW, they commented that in at least 75% of cases, they would encourage someone to consider being more active.
Without fail, every single SPLW interviewed, commented that roughly 90% of the people they support are preoccupied with issues of debt, concerns about housing tenancies, relationship issues, unemployment and underlying anxiety or mental health issues. All felt that the greatest support they could provide was to help find, and then link the patients into an appropriate service or process to help them come to terms with or resolve those issues. Against this backdrop (and with increasing pressure to be more productive perhaps), it is important to recognise that the opportunity and the skillsets required to motivate these individuals into increased levels of activity are under pressure.
The core question might be how likely it is that an process will result ultimately in a prolonged behaviour change in relation to increased exercise. Beyond the individual estimates (as the data is not recorded accurately at all), there was one GP who kept a more robust set of information; over a two-year period, he tracked how successful he was at encouraging patients to join the . The result was that he was successful 20% of the time to persuade people to attend at least once; this is someone with great skill and experience, with significant passion for the Park Run and who was targeting the recommendation at people who he was confident would benefit. Over those 2 years, the GP will have delivered over 13,000 appointments that resulted in believing that the Park Run was relevant for 300 people and of those 20% (or 60) ultimately attended. This in effect is a success rate of under 0.5%.
@SPLW
Obviously, a GP has a much broader role, but actually the similarity to the real impact that a SPLW could be similar. Most link workers estimated that about 20% of the time that they recommend anything, then someone would take it up; this is across the board to any community service, be that taking up exercise or getting financial / benefits advice for example.
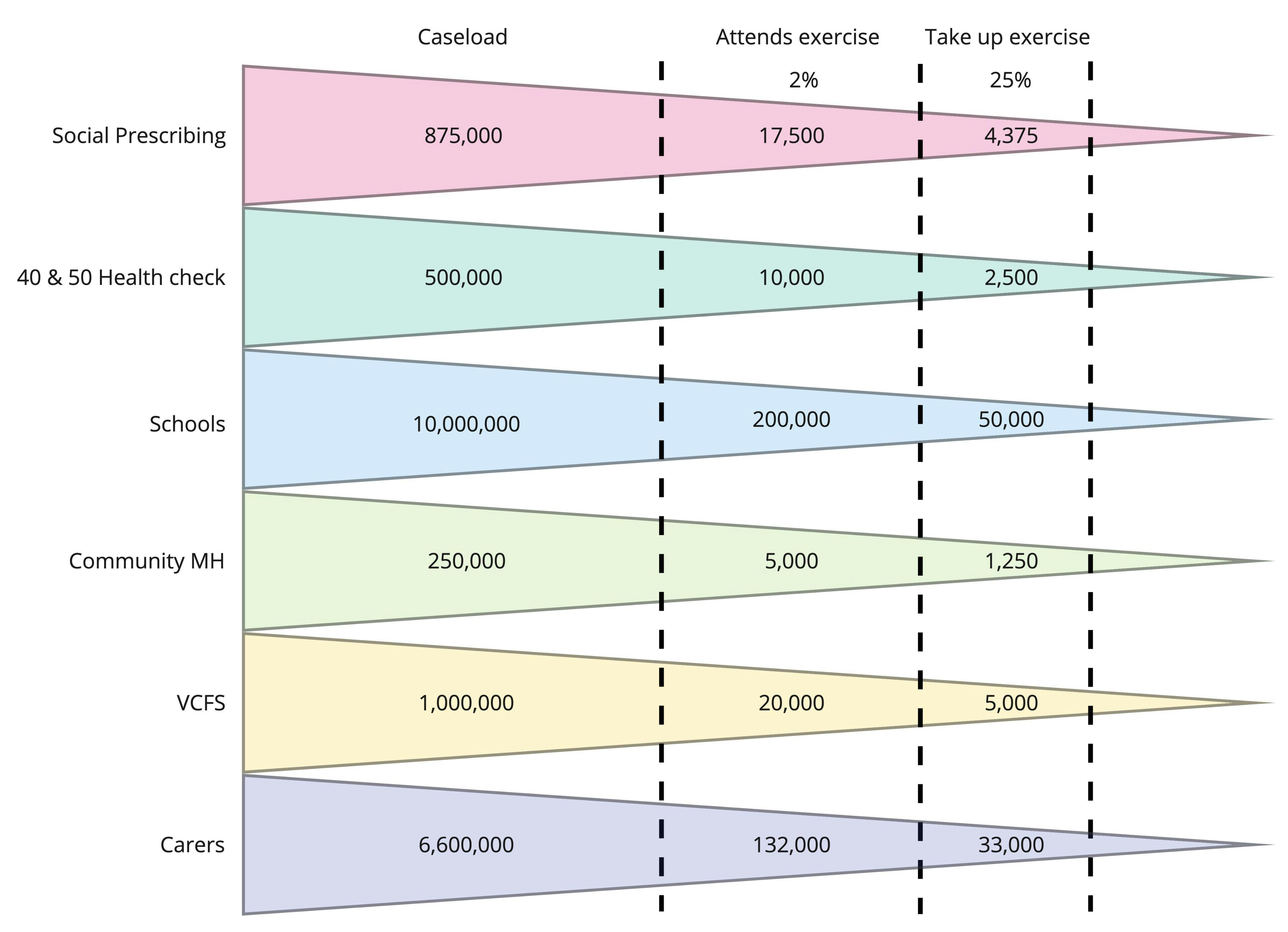
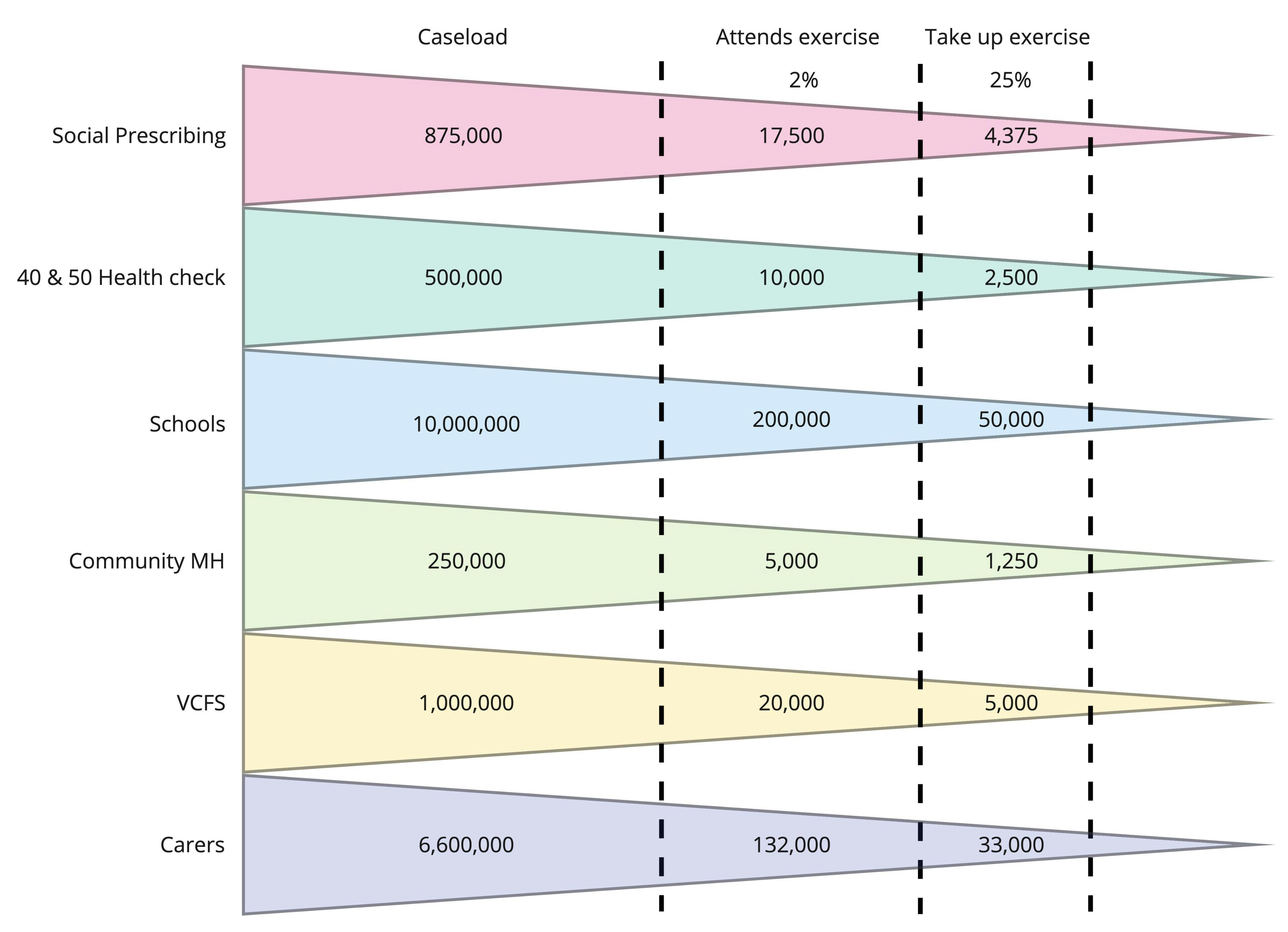
The range may therefore be that between 0.5% and 2% of all caseloads may take up exercise once. If the assumption is that 25% of these people take it up sustainably, then the table below offers some indications about the impact that Social Prescribing Link Workers may have on increasing take up of exercise. There are a huge number of factors that will influence these variable outcomes, not least age, underlying conditions or situation, cultural attitudes / beliefs and location; as well as recognising that the starting position of every SPLW will differ in terms of their own beliefs, confidence and skills in having these types of conversations.
@SPLW
Referral take up funnel
There are no rows in this table
It is easy to debate whether these figures could be higher or lower. The view of the researchers, admittedly based upon a small sample size of data and on anecdotal data, is that right now the number of people being supported through the process to take up exercise on a sustainable basis will be nearer 400 than 4,000. Against the current total volume of Social Prescribing patients supported per annum, there is theoretically significant opportunity for some increase against this baseline.
Furthermore, based upon light-touch research admittedly, it is interesting to note that generally there is some scientific evidence for exercise having a positive impact upon health outcomes for precisely the cohort of people that tend to be supported currently by ; those with Mental Health concerns. The scientific evidence for the impact of exercise on weight, for example is not very robust, whereas the scientific evidence for the impact of exercise on mental Health is fairly good. This certainly, theoretically if not necessarily financially, strengthens the case for the need to invest in the right motivation skills and time to encourage this cohort to consider exercise for their own improved health.
@SPLW
A broader perspective on Social Prescribing
There is a certainly, therefore, a theoretical case to be made that there is an opportunity to improve the use of Open Data within GP-referred cases to deliver an increase in the volume of referrals into exercise. Whether there is a financial return on any investment is less evident, let alone exploring to whom the costs should fall to deliver the changes. There will need to be significant investment into cultural and process change, as well as investment into making Open Data and the supporting technology a reality.
@SPLW
However, similar to the approach adopted by , any work looking at the use of Open Data within GP-led Social Prescribing, should consider simultaneously the broad range of other community referral processes, many of which have higher volumes of cases. Perhaps more importantly, some may also target / find people earlier in the development of any underlying health issues. This is important for a number of reasons:
The following table, therefore, sets out some other potential referral processes that could also be targeted as opportunities to promote the adoption of Open Data in the same way, alongside processes. The information about the volumes and types of processes is exemplary only, rather than including all areas, but provides an overview of potential areas to consider.
@SPLW
Referral Process
There are no rows in this table
Many of the recommendations that are being made for changes to the data standard and the tooling (to ensure additional information is available to answer the issues for the cohort) would apply equally to most of these referral pathways. Similarly, it is likely that many of the actual patients being supported by SPLW may well also be receiving support from other community-based professionals and support services; having two professionals advocating similar messages may increase the likelihood of lasting behaviour change.
@SPLW
Looking at this same argument from an alternative perspective, the highly disjointed and variable approach to Social Prescribing indicates that the model remains immature and overly-generic. There may be significant value from a wholesale re-design of specific pathways that cross the cohorts and referral pathways above. In support of this, there may also be some benefit here in creating some that can identify the holistic types of exercise and non-exercise opportunities that may be appropriate for typical clients groups such as:
@SPLW
@ASD
In summary, any further investment or next steps to drive accelerate the adoption of open data might consider the following:
@SPLW
The final consideration is that the approach to increasing exercises referral into Social Prescribing should look to position a holistic approach, for the following three reasons:
@SP
@OpenActive
@SP
Different Measurements Tools Used
There is a range of different measurement tools being used within Social Prescribing and often multiple tools being used in the same sets of reporting. The measures identified are:
Measurement tools
There are no rows in this table
What was less clear is exactly how and why the different measurement tools are being used. The capture and submission of data to CCG commissioners seemed to be an accepted process, with fairly limited understanding of why the information is collected, who would use it and the types of improvements / decisions that they were seeking to make. The paragraphs below, offer some consideration of what might be measured beneficially by which sets of roles and using what sets of information.
The core function role of is to link someone with non-medical support within their own community. In this context, the key things that arguably should be measured are:
@SPLW
However, all of the measurements that are currently captured tend to focus on whether someone is reporting some improved sense of well-being. It is important to recognise that these measures are about all interactions and hence cover cases where people may have been linked with services covering an enormous range of offers from benefit assessments, to befriending services to singing groups and including walking groups and more structured physical activity. The purpose of the information collected was not clear always to people interviewed, however, significant caution is recommended where the information may be considered as evidence to evaluate the “success” of Social Prescribing or the “success” of a particular service. The following provides some examples of the potential risks with using the information collected to make evaluation judgements:
@SPLW
@SPLW
It is certainly true, however, that there is a need for evaluating the broad Social Prescribing model, where the total resource invested in the current 12-month period may be in excess of £100 million (where overheads, management costs across the 1250 , contract costs with the providers and software costs are included). It is notoriously complex to measure and evidence the success of preventative expenditure. The following provides some areas for consideration:
@PCNs
@SPLW
The view of the report authors is that the continued collection of such a breadth of information seems misplaced. The focus should be upon the performance of the SPLW process (how many people are being supported, how many actually take up a referral, and what is the quality feedback on the SPLW support). Measuring and monitoring this information locally will help improve the SPLW process; the SPLW support provided is undoubtedly highly valued as a linking / referral step into community support. There does remain a question to consider, which is whether the role of the SPLW is as a befriender / counsellor, or as a link worker into someone else who provides the befriending / counselling role. It is this question that needs to be considered, but this is refining the existing set-up to improve it, rather than wholesale change of something that can play an important role in the broad health prevention strategy.
Download the PDF version
Numbers and Measures.pdf
1.5 MB
Want to print your doc?
This is not the way.
This is not the way.
Try clicking the ··· in the right corner or using a keyboard shortcut (
CtrlP
) instead.