Skip to content
The Design
 Limitations & Future Work
Limitations & Future Work
Overview
Motor Selection Re-evaluation
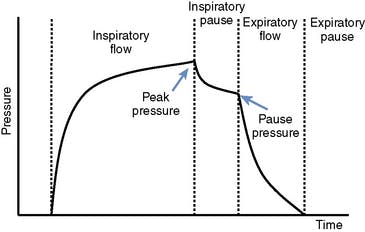
Pressure Sensor Data Collection
PCB Development
Battery Addition
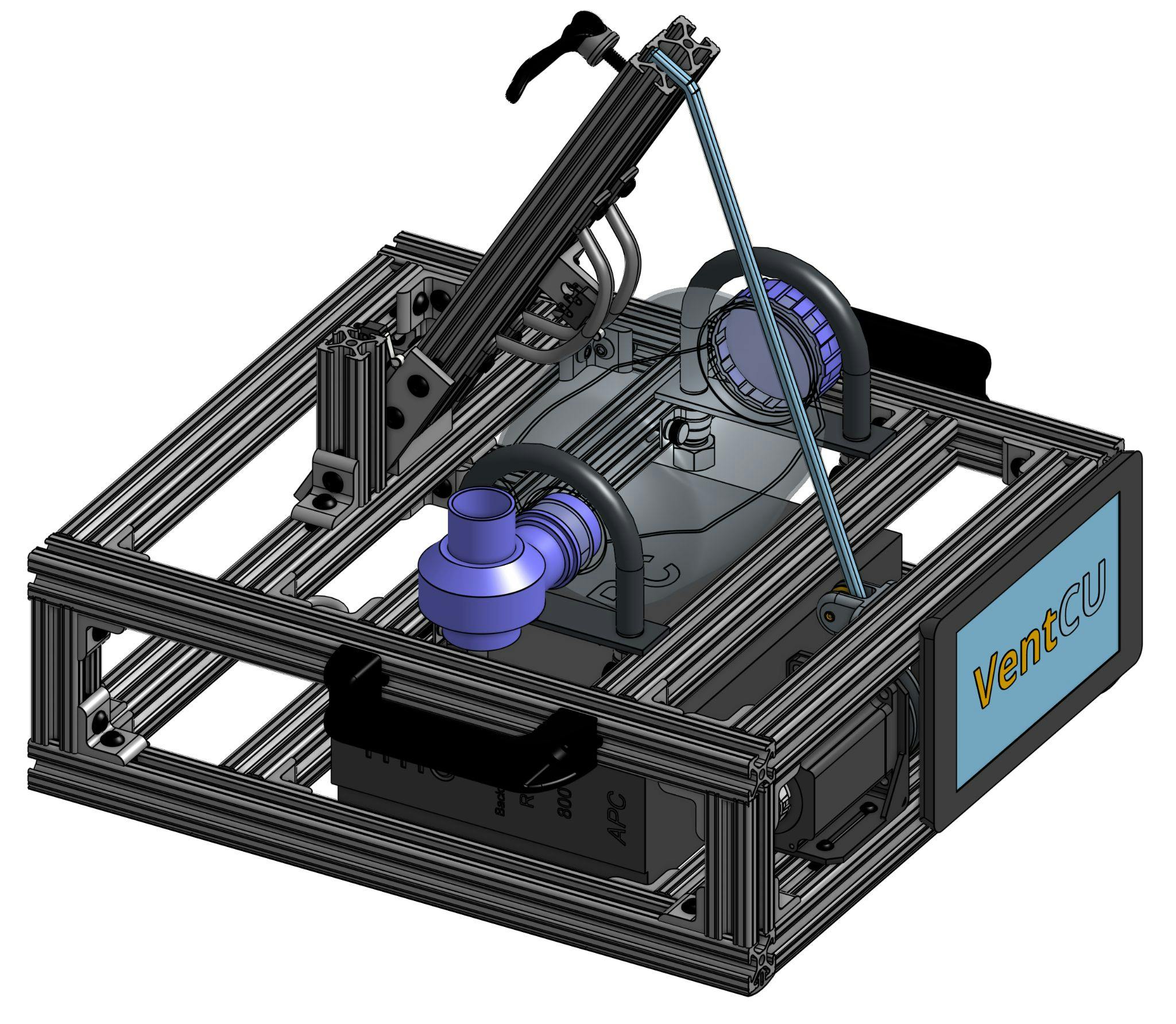
Control System
Next: |
Want to print your doc?
This is not the way.
This is not the way.

Try clicking the ⋯ next to your doc name or using a keyboard shortcut (
CtrlP
) instead.